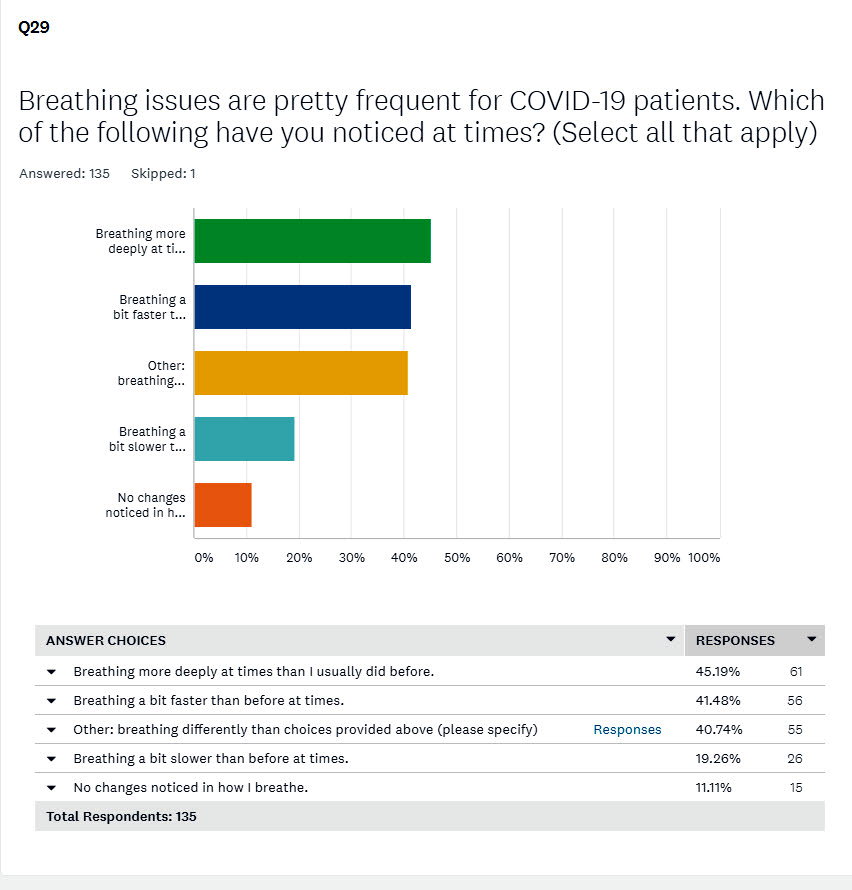
Q. 29 - Breathing issues, breathing differently
LTCOVID.com
Thanks for visiting!
To translate this page, select your
language from the dropdown menu below:
"Breathing problems" are clearly frequent for those with "long-term" COVID-19.
The fact that 41% of respondents felt compelled to elaborate on the suggested completions speaks to this.
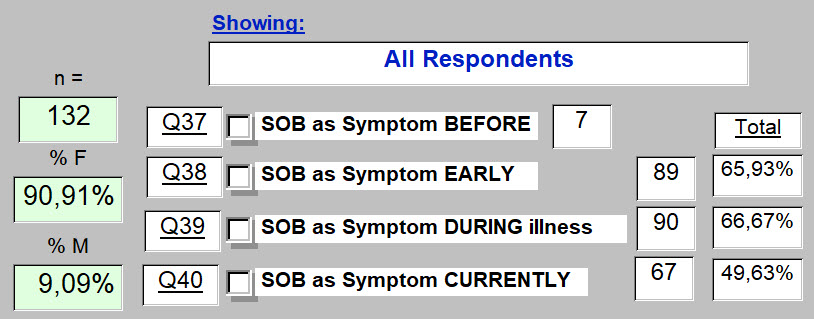
We will also see in subsequent questions that "shortness of breath" is not only frequent, it tends to persist throughout the illness, as shown below for this sample.
Essentially 2/3rds have Shortness of Breath (SOB) as a symptom during most of the duration of the illness, and at the time of completing the questionnaire, half still suffered this symptom.
70.4% felt that their respiratory system had been affected during the illness.
While the cardiovascular system can also be responsible for shortness of breath, respondents felt this to organ system be less commonly involved (58.5%) than the respiratory system. We accept that these are primarily distinctions made subjectively.
Breathing more deeply and more rapidly than before becoming ill are the two primary choices selected.
These may be taken as the hallmark of hyperventilation. While anxiety is frequently associated with hyperventialtion, and while changes in pCO2 are primary determinants of minute ventilation, the low peripheral oxygen levels documented by many in this illness may be a contributor. Primary involvement of this viral illness with the respiratory system, abnormal findings clinically, and pathologic findings at autopsy, need not be presented more completely here.
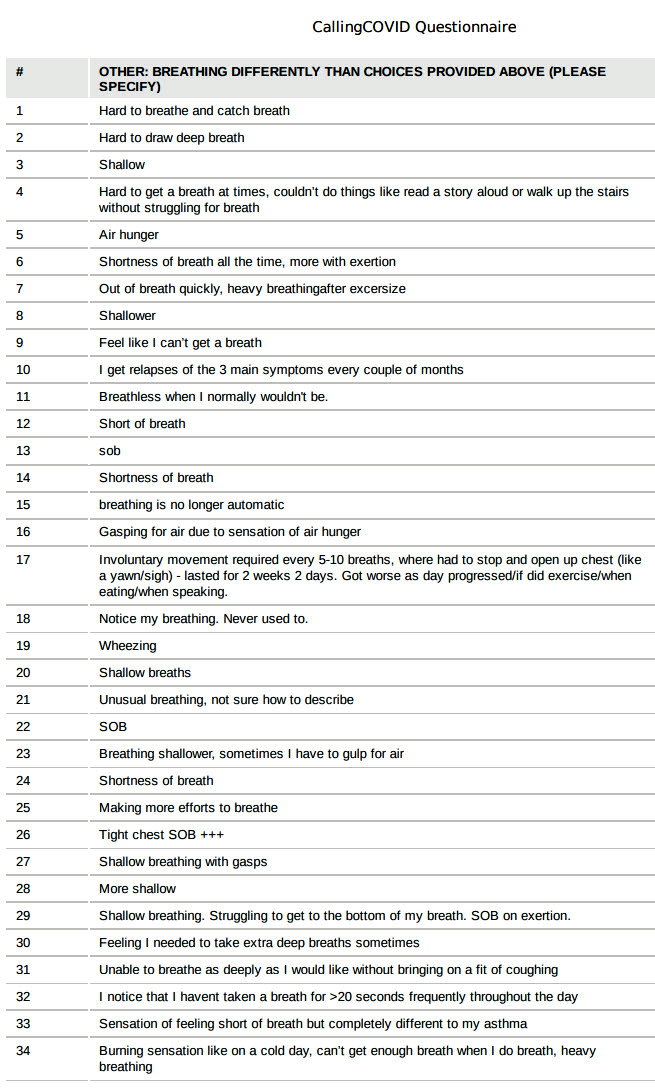
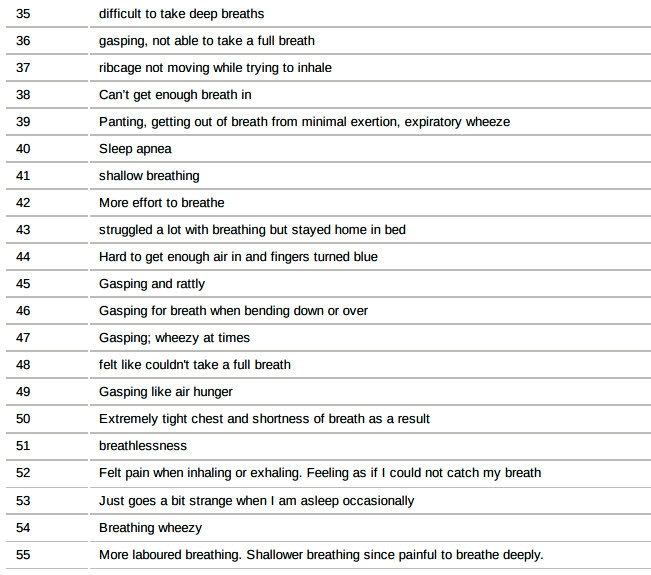
But here is a list of additonal findings as added by 55 respondents. There are some duplicates of course. Shortness of breath appears frequently, and helps get the message across. But these are the additional words that these respondents wanted to get across :
Clearly, dysfunction of the respiratory system has caught the attention of these respondents, representing a major source of disability.
Only one skipped this question. Fifty-five (40.7%) felt a further need to clearly explain what they experienced as they breathed.
Hyperventilation, breathing more deeply and/or more rapidly, as findings often accompanying anxiety or panic attacks was mentioned.
Does that explain what these respondents are living with throughout most of this unfortunate illness?
The question is phrased in this way to introduce the error of seeing such an illness through a portal that permits only one choice: ("This is a physical illness") or the other ("This is an emotional illness").
We will see through the responses to subsequent questions that such a dichotomous approach is taken almost as frequently by those suffering this illness, as by those charged with helping them to find a way through it. That always makes it more difficult to find an approach that works.
As we shall see through the presentation of results for questions that follow, it is both. Both physical and emotional components have been clearly defined by these respondents.
And how could it be otherwise?
There may also be a bias that if the physical part could just be made better, that the emotional part would take care of itself. That may not be guaranteed.
A related and critical point, also explored in the questions that follow, is left here as a question. Has the response to this illness been as effective in its pursuit of both undeniable components present in "long-term" COVID-19 : Effective therapy for both physical and emotional components?
Electing to pass through a polarizing portal, unfortunately does not lead towards a total therapeutic approach that can be as fully effective as it might be otherwise, and as this challenging illness requires.
<<<< Previous page
A découvrir aussi
- Q.5 : Gender
- Q. 43 - The perceived balance between Physical & Emotional components of the "long-term" COVID-19 illness
- Q. 53, 54, 55 - Quality of Life and "long-term" COVID-19